Experts reveal failures in male infertility diagnosis are driving unnecessary IVF
A new study attributes 50% of infertility cases to male factors, yet this issue is often overlooked due to poor understanding
According to a recent study, many couples are undergoing unnecessary and costly IVF treatments because male fertility is under-researched by the healthcare system.
Primarily, misinterpretation among GPs and a lack of specialists and NHS testing means male fertility is often overshadowed in couples struggling to conceive, despite men accounting for 50% of all infertility cases.
Meanwhile, several causes of male fertility can be treated. One of the most common reasons is a varicocele-an enlargement of the veins in the scrotum that increases testicular temperatures, which damages sperm and can be treated through surgery.
In this connection, Vaibhav Modgil at the University of Manchester said there was a lack of understanding of male infertility which ultimately affects 5% to 10% of men in the UK.
Experts urged that the government’s first men's health strategy would contain a tactical focus on male infertility similar to Australia’s.
Fertility has been historically considered a women’s health issue, and more rigorous scrutiny needs to be done to scrutinize the lifestyle and medical history of both the partners.
The National Institute for Health and Care Excellence has reportedly taken a significant step in updating its guidelines to recommend more testing for men.
Recent research from Fertility Action established that 80.6% of GPs had received no education on male fertility, and that 97% would not be able to analyse accurately for varicocele.
The concept of male fertility has long suffered to achieve proper recognition as a health issue.
It is a bold step for shaping our ways of thinking and acting on men’s health and adapting as challenges emerge with time.
The recent study suggests that the primary goal is to ensure all couples are given the chance to conceive naturally, before committing to the journey of reproductive technologies.
Nonetheless, the latest advancement underscores the fact that we must invest in the proper diagnosis, and serves as a strong foundation for improving how we think about men’s health.
-
Imagine Dragons star, Dan Reynolds recalls 'frustrating' diagnosis
-
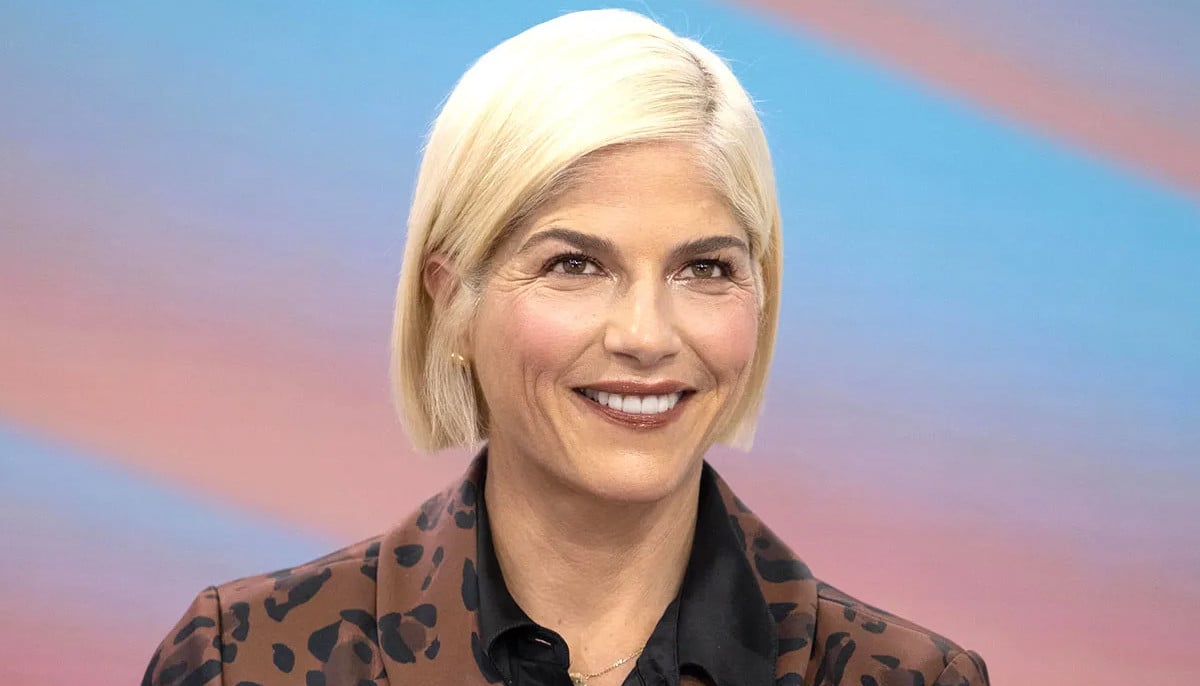
Selma Blair explains why Multiple Sclerosis 'isn't so scary'
-
Can brain stimulation make people kinder & less selfish? New study offers hope
-
Mariah Carey details 'hardest' bipolar disorder experience
-
Pink reveals health routine for asthma management
-
Gigi Hadid talks about 'relieving tension' amid having Hashimoto's disease
-
Selena Gomez explains why she thought lupus was 'life-or-death'
-
How Kim Kardashian made her psoriasis ‘almost’ disappear