New research answers why anti-depressants don’t work for so many patients
Researchers have uncovered a more effective line of treatment for depression
Depression is one of the most common mental health conditions around the world. Millions of people live with ongoing sadness, low energy, sleep problems, and loss of interest in daily life.
For many, antidepressant medicines are the first treatment offered and these drugs are widely used and help many people.
However, a large number of patients try one medication after another and don’t feel any significant improvement in their condition. Until now, doctors have not fully understood why this happens so often.
A major new study from the University of Sydney’s Brain and Mind Center offers an important explanation to the question.
The research suggests that depression is not a single illness, but a group of different conditions that may need different line of treatments and the study focused on identifying a specific type of depression that does not respond well to standard antidepressants. This finding could change how depression is treated in the future.
The research team studied data from nearly 15,000 Australians who had experienced depression. This made it one of the largest studies of its kind.
The data came from the Australian Genetics of Depression study, which collects detailed information about symptoms, health history, and genetics.
About three quarters of the participants were women, reflecting the fact that depression is more commonly diagnosed in females.
When researchers looked closely at the data, they found that around 21 percent of participants shared a pattern of symptoms that stood out clearly from the rest. This group was identified as having what researchers call “atypical depression.”
People in this group showed different symptoms compared to what is usually seen in depression. Instead of losing weight and sleeping less, many reported gaining weight and sleeping much more than usual during their worst depressive periods.
They often felt heavy, tired, and slow, both mentally and physically. These symptoms can deeply affect daily life, work, and relationships.
Most importantly, this group did not respond well to common antidepressants such as SSRIs and SNRIs. These drugs work by changing levels of certain brain chemicals.
For people with atypical depression, these medicines were often ineffective and more likely to cause side effects such as weight gain. This can make people feel worse, not better, and may lead them to stop treatment altogether.
Lead researcher Dr. Mirim Shin explained that people in this group showed higher genetic risk linked to metabolism, immunity, inflammation, and sleep timing. This meant that their depression may follow a different biological pathway. If this is true, it helps explain why standard treatments often fail and why side effects of anti-depressants are more common.
This research strongly supports providing personalized mental health care to patients rather than using the same treatments for everyone, doctors could one day choose therapies based on a person’s biology, symptoms, and overall health.
This could reduce long periods of trial and error, lower the risk of side effects, and help people recover faster.
And while more research is needed, this study marks an important step towards more accurate diagnosis and better care for people with depression.
-
Can brain stimulation make people kinder & less selfish? New study offers hope
-
Mariah Carey details 'hardest' bipolar disorder experience
-
Pink reveals health routine for asthma management
-
Gigi Hadid talks about 'relieving tension' amid having Hashimoto's disease
-
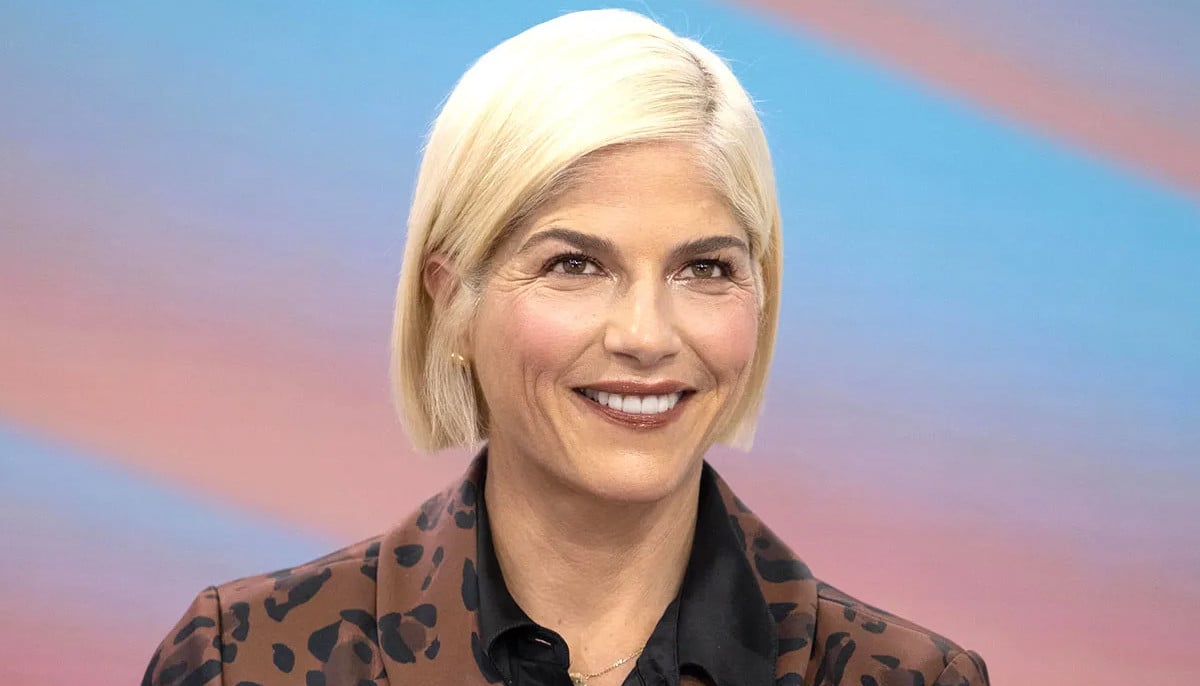
Selena Gomez explains why she thought lupus was 'life-or-death'
-
How Kim Kardashian made her psoriasis ‘almost’ disappear
-
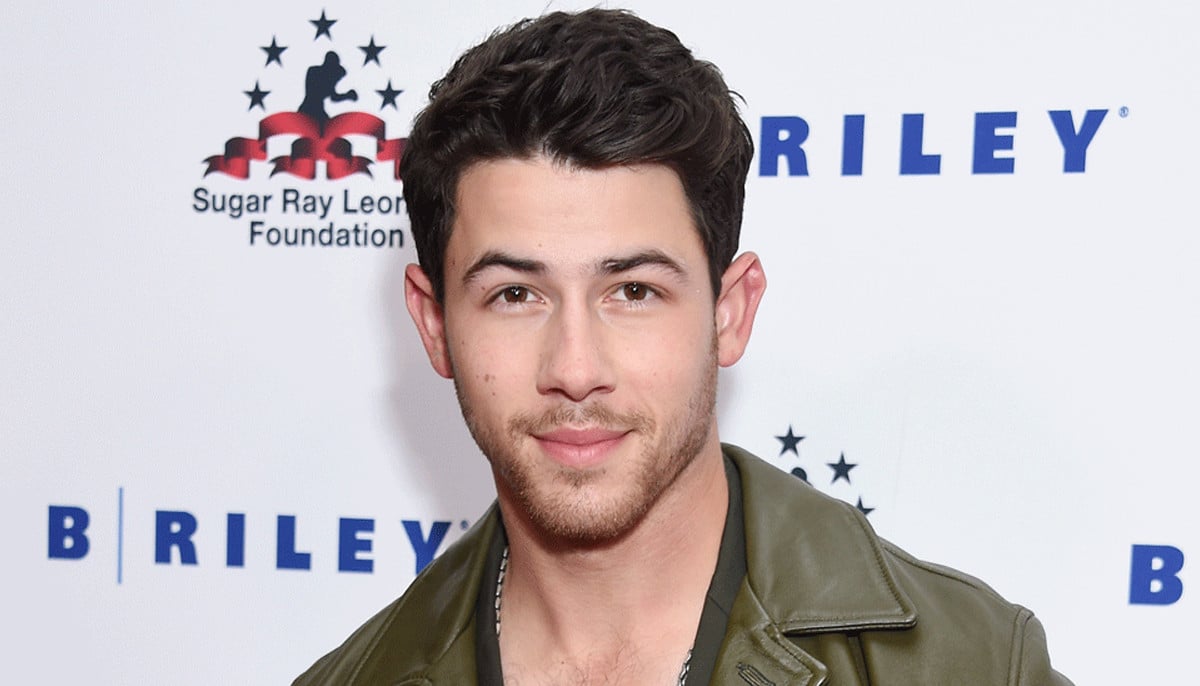
Nick Jonas gets candid about his type 1 diabetes diagnosis
-
Sir Jackie Stewart’s son advocates for dementia patients