Blood pressure medication linked with suicide risk? New study explains
Blood pressure medications are considered safe for most patients but a new study has raised questions
Blood pressure medicines are among the most commonly prescribed drugs in the world. Millions of people take them every day to protect their hearts, kidneys, and blood vessels.
These medicines are usually seen as safe and effective, and for most people, they are. However, a new study has raised concerns about a possible link between one type of blood pressure medication and an increased risk of suicide.
The study was carried out by researchers at St. Michael’s Hospital in Canada and was published in the medical journal JAMA Network Open.
The researchers focused on two widely used types of blood pressure drugs: angiotensin receptor blockers, known as ARBs, and angiotensin-converting enzyme inhibitors, known as ACE inhibitors.
Both drugs are commonly prescribed for high blood pressure, heart failure, chronic kidney disease, and diabetes.
These two types of medication work on the same hormone system in the body, called the renin-angiotensin system.
This system helps control blood pressure by tightening or relaxing blood vessels. A hormone called angiotensin II plays a key role. When there is too much angiotensin II, blood vessels narrow, and blood pressure rises.
ACE inhibitors lower blood pressure by reducing how much angiotensin II the body makes while ARBs work differently.
Instead of reducing the hormone, they block it from attaching to blood vessels, stopping the vessels from tightening. Both approaches lower blood pressure, but they affect the body in slightly different ways.
To explore whether these differences might matter for mental health, the researchers examined large Canadian health databases. They looked at 964 people who died by suicide within 100 days of starting either an ARB or an ACE inhibitor.
These individuals were compared with more than 3,000 similar patients who were taking the same types of medication but did not die by suicide.
After carefully comparing the two groups, the researchers found a concerning pattern. People taking ARBs had a 63 percent higher risk of suicide than those taking ACE inhibitors.
This finding remained even after the researchers adjusted for age, gender, and other health conditions.
The study does not prove that ARBs cause suicide, but it suggests there may be a connection that deserves closer attention.
One possible explanation involves how these drugs affect the brain. Angiotensin II does not only work in the heart and blood vessels. It is also active in the brain, where it may influence mood, stress, and emotional regulation.
The researchers believe that blocking angiotensin II in the body with ARBs might lead to higher levels of this hormone in the brain.
Increased angiotensin II activity in the brain has been linked in earlier research to anxiety, depression, and stress responses. This could potentially increase the risk of suicidal thoughts in vulnerable individuals.
The lead author of the study, Muhammad Mamdani, emphasized that this research is an early warning and not a final answer.
He explained that patients should not stop taking their blood pressure medication based on this study alone. Stopping medication suddenly can be dangerous and may increase the risk of heart attack or stroke.
-
Sarah Ferguson’s dual cancer journey
-
Demi Moore was left with ‘intense’ illness after ‘The Substance’
-
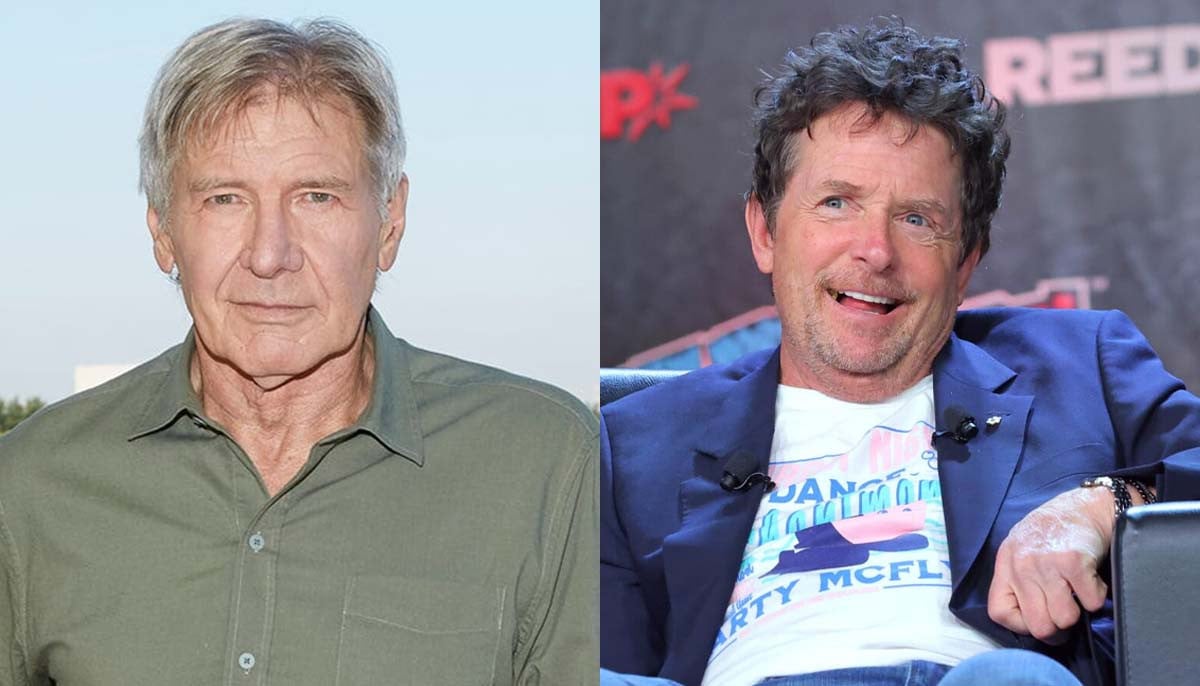
How Michael J. Fox helped Harrison Ford with his Parkinson's monologue
-
‘Stranger Things’ star Gaten Matarazzo reveals how cleidocranial dysplasia affected his career
-
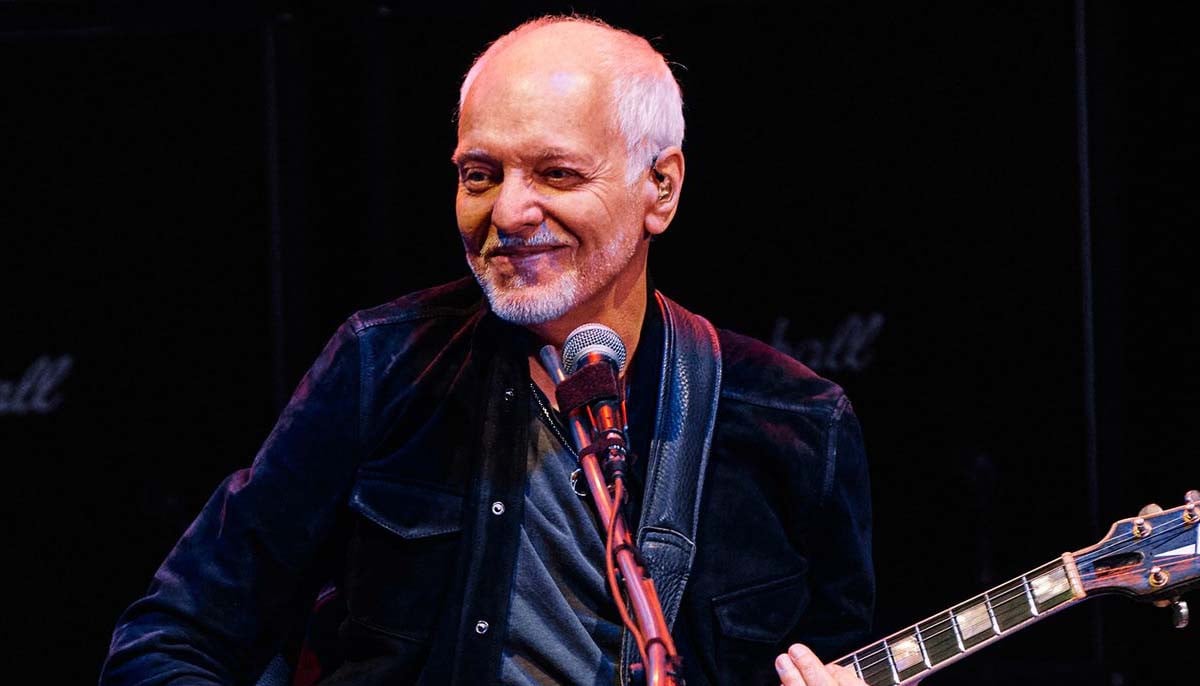
Peter Frampton details 'life-changing- battle with inclusion body myositis
-
How does Sia manage 'invisible pain' from Ehlers-Danlos syndrome
-
Halsey mentions how she 'gained control' over endometriosis condition
-
Shia LaBeouf sent to rehab for not taking ‘alcohol addiction seriously’