New study reveals routine blood test may help detect undiagnosed osteoporosis risk
A common measured enzyme could be used as an early indicator of hidden osteoporosis risk
According to a new study published in the journal Frontiers in Endocrinology, researchers have found that a commonly measured enzyme in routine blood tests, Alkaline Phosphatase (ALP) could serve as a marker for osteoporosis.
The study demonstrated that higher ALP levels were consistently linked to a greater likelihood of osteoporosis, with stronger associations among metabolically younger female women.
The significant need for accessible biomarkers
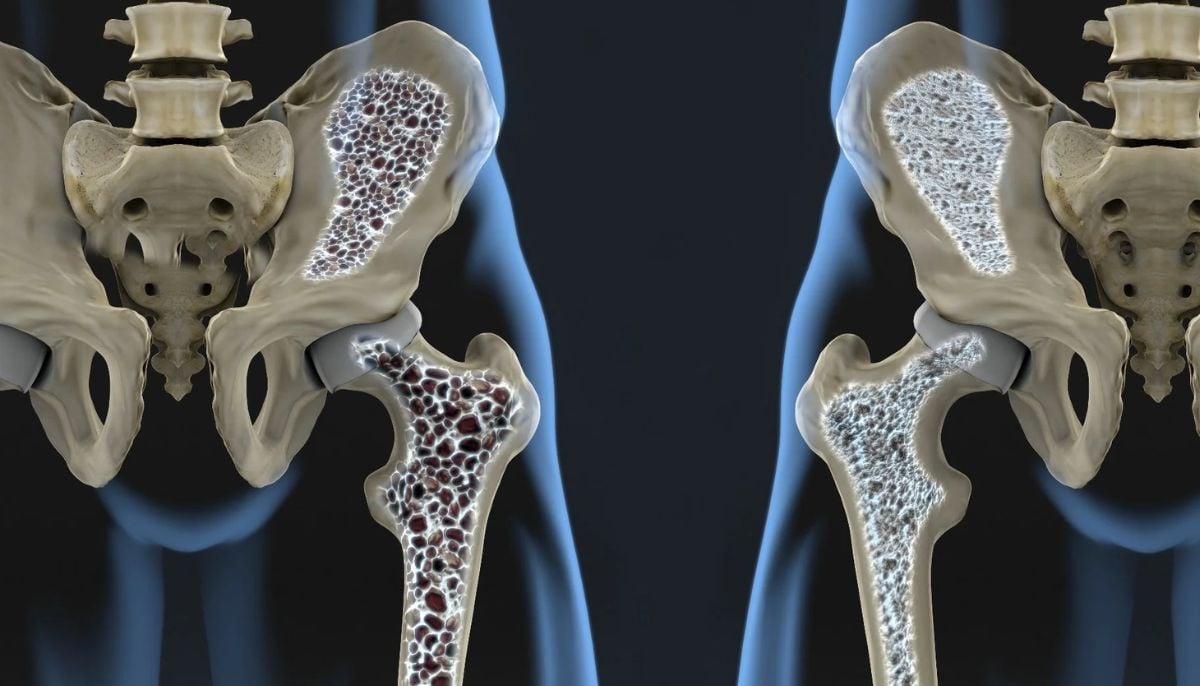
Osteoporosis is characterized by narrowing bone mass and structural deterioration, leading to an increased risk of fractures and substantial impacts on health and quality of life.
It has been observed that as fracture sharply increases with age, especially after 75, there is growing interest in identifying accessible biomarkers that can detect bone loss earlier.
ALP, produced primarily by bone-forming osteoblasts and hepatocytes has a crucial role in bone mineralization by degrading pyrophosphate.
ALP is cheap and available in routine health checks, and researchers have explored its potential as a biomarker of bone health.
Researchers have specifically analyzed whether total ALP can indicate osteoporosis risk in a large, systematically assessed population.
Eligible participants were adults aged 20 or older who had completed ALP testing and dual-energy X-ray absorptiometry (DXA) scans of the hip and spine.
It has been observed that hospital procedures were used to collect anthropometric measurements, blood pressure, ultrasound findings, and biochemical markers, including glucose, lipids, uric acid, and liver enzymes.
While among 12, 835 participants, 9.5% were diagnosed with osteoporosis, and nearly all individuals had ALP levels within the clinical reference range. Participants with osteoporosis had elevated ALP levels.
Subgroup disparities and metabolic influences
Subgroup analysis demonstrated stronger statistical associations rather than higher risk in women, younger individuals, and those with normal liver enzymes and healthier metabolic profiles.
The moment when liver enzymes were increased, or when glucose or lipid profiles were abnormal, the link disappeared while suggesting that metabolic and hepatic factors may disrupt the association between bone status and ALP.
This research study has analyzed that higher serum total ALP is closely associated with a greater likelihood of osteoporosis.
The association was strongest in younger women and metabolically healthy individuals because ALP more accurately depicted ALP when liver function and metabolic status are normal.
Nonetheless, the study strengths include the standardized clinical data, and detailed subgroup analysis.
The study has not included information on physical activity, thyroid status, medication use, and diet which limit the findings.
In addition, it may serve as a provisional limit for further assessments of bone health, though longitudinal cohort studies are required to substantiate its causal and predictive estimation.
-
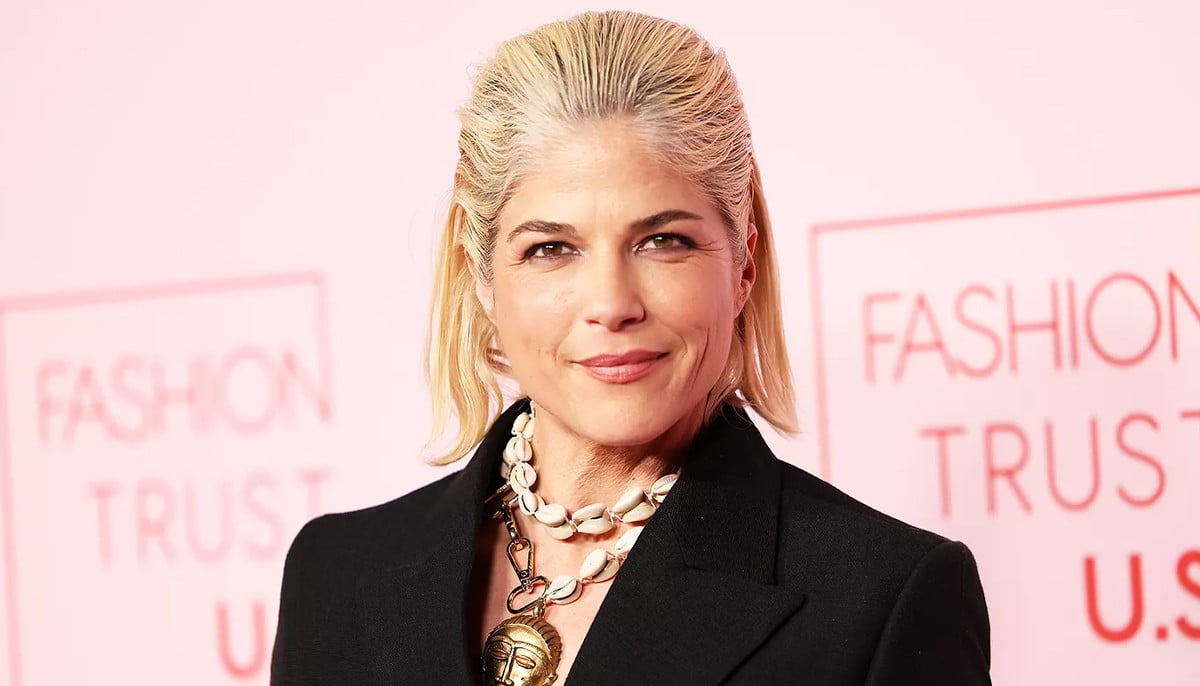
Jada Pinkett Smith details how her memoir combats 'shame' around alopecia
-
Billy Joel admits cancelling of tour due to brain disorder 'sounds a lot worse' than it is
-
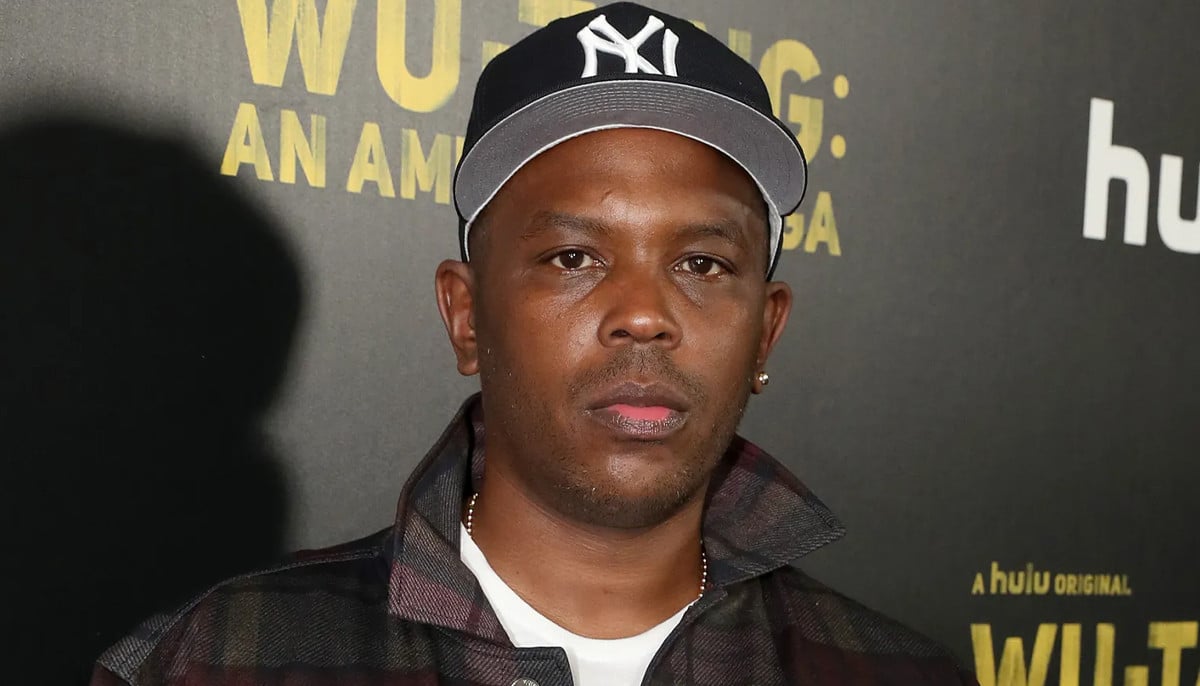
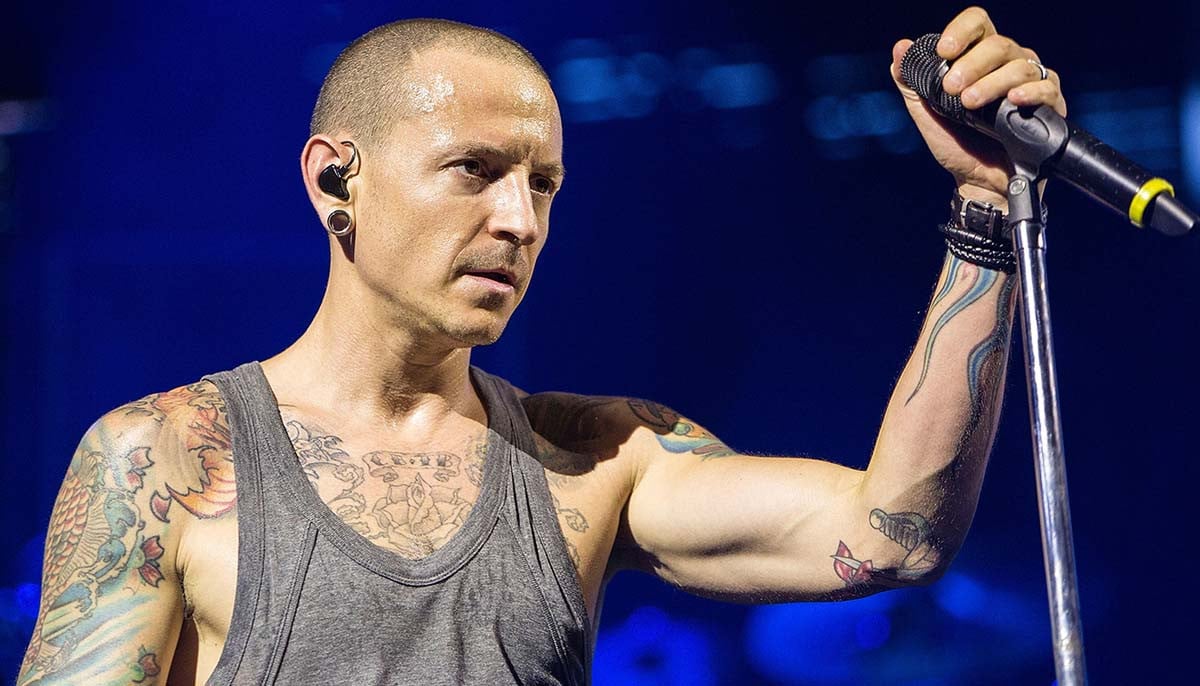
Chester Bennington’s mental health story and lasting legacy
-
Yerin Ha opens up about shocking diagnosis post ‘Bridgerton’ season 4
-
Everything to know about Justin Bieber's facial paralysis
-
Sarah Ferguson’s dual cancer journey
-
Demi Moore was left with ‘intense’ illness after ‘The Substance’
-
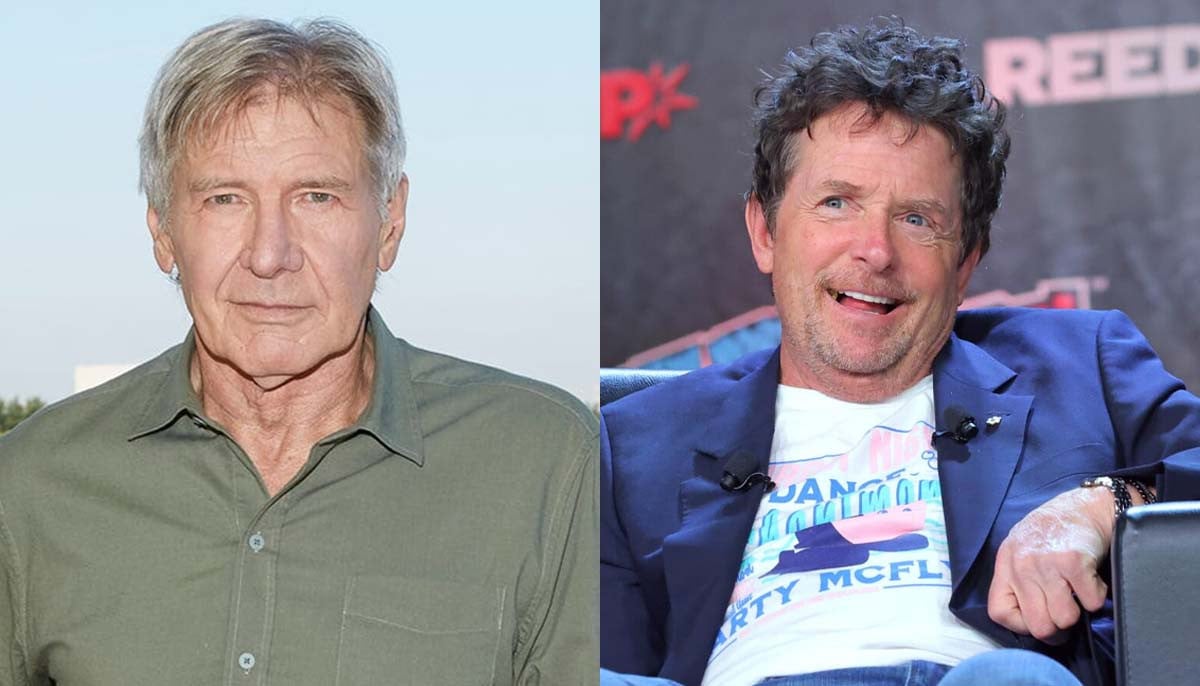
How Michael J. Fox helped Harrison Ford with his Parkinson's monologue