New study reveals 11 genetic loci linked to impulsive decision-making
The recent genome-wide association study has successfully identified genetic loci and the reasons those patterns are linked to various factors
A recent study published in Molecular Psychiatry has successfully identified 11 independent genetic loci linked to delay discounting (DD).
Primarily, it scrutinized how these variants influence physical, behavioral, and neuroimaging traits linked to both physical and psychiatric health results.
What is DD?
DD is primarily inclined to choose immediate, smaller rewards over delayed but substantial rewards. It is a heritable trait associated with distinct disorders signalized by impaired impulsivity and decision-making.
On the contrary, obsessive-compulsive disorder is associated with lower DD.
How was the study conducted?
The researchers measured DD using the intertemporal choice. This curve is precipitous when immediate gratification is preferred, as compared to a flat trajectory.
A previous genome-wide association study (GWAS) provided genetic data for 134,935 participants of the 23andMe cohort, all of them of European ancestry.
The study analyzed both global and genetic linkage between DD and health outcomes; network analyses were used to scrutinize the distinct molecular pathways involved in these processes.
Meanwhile, multi-dimensional analyses were used to analyze genetic factors that are unique to DD compared to those shared with other intellectual qualities such as educational attainment, intelligence, and executive functions.
Study findings revealed 93 unique DD-associated genes
The GWAS analysis revealed eleven significant loci containing 93 unique DD-associated genes, 20% of which were located within the ch16p11.2 GWAS locus.
The recent analysis is distinctive from previously reported association with the chromosomal locus rs6528024 (chrXq13.3).
Results demonstrated that observed genetic variants were single-nucleotide polymorphisms (SNPs) that explained 9.9% of the differences in DD between individuals.
It has been observed that most of the SNPs were present in loci previously associated with enterprising, substance abuse, and psychiatric illness.
DD is primarily associated with 73 psychiatric, physical, and cognitive traits. A subset of these correlations continued to be notable for shared genetic influences with cognitive traits including education, intelligence and executive function.
Metabolic pathways shared between DD and BMI also overlapped with those associated with schizophrenia, externalizing behaviors, and educational attainment.
Study conclusions and paving the way for future revelations
The current study used a five-fold sample than the work done by previous workers. However, eleven genetic loci, including 93 genes, were found to be closely associated with DD risk.
The study underscores a higher predisposition to DD that reflects shared biological pathways that overlapped with cognitive operation, psychiatric conditions such as depression and metabolic health consequences.
Nonetheless, future work will contribute to expanding PheWAS performance to a non-European cohort because the PGS developed on European data becomes inaccurate in populations with different ancestries.
-
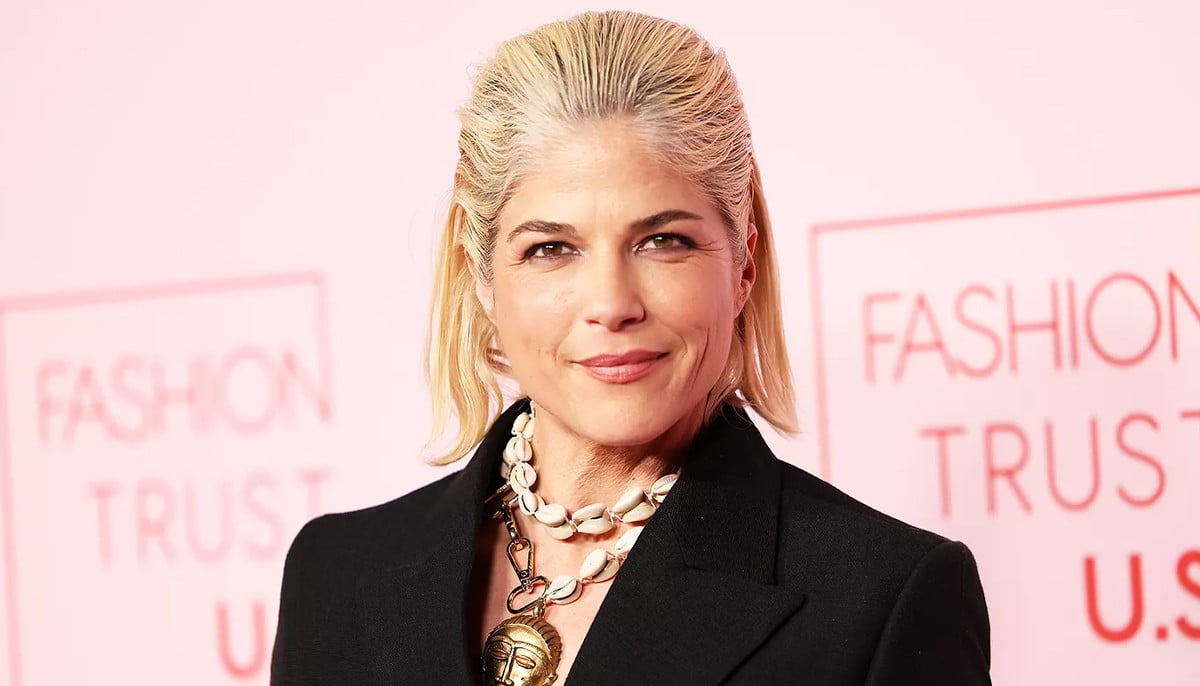
Jada Pinkett Smith details how her memoir combats 'shame' around alopecia
-
Billy Joel admits cancelling of tour due to brain disorder 'sounds a lot worse' than it is
-
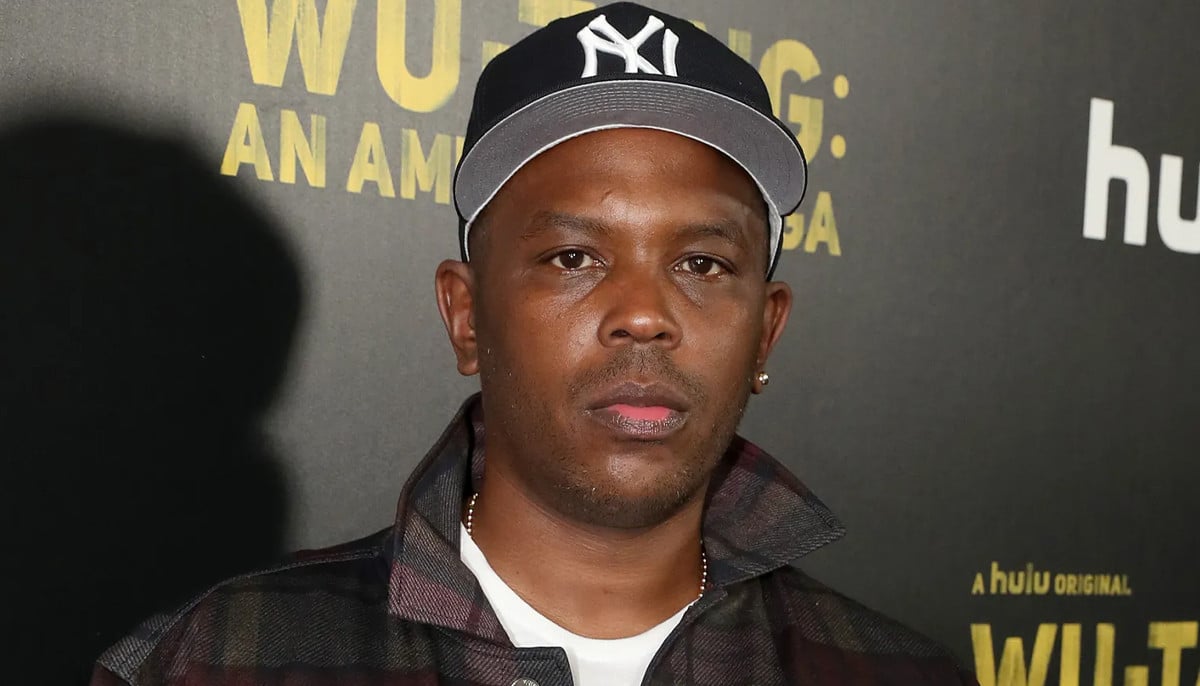
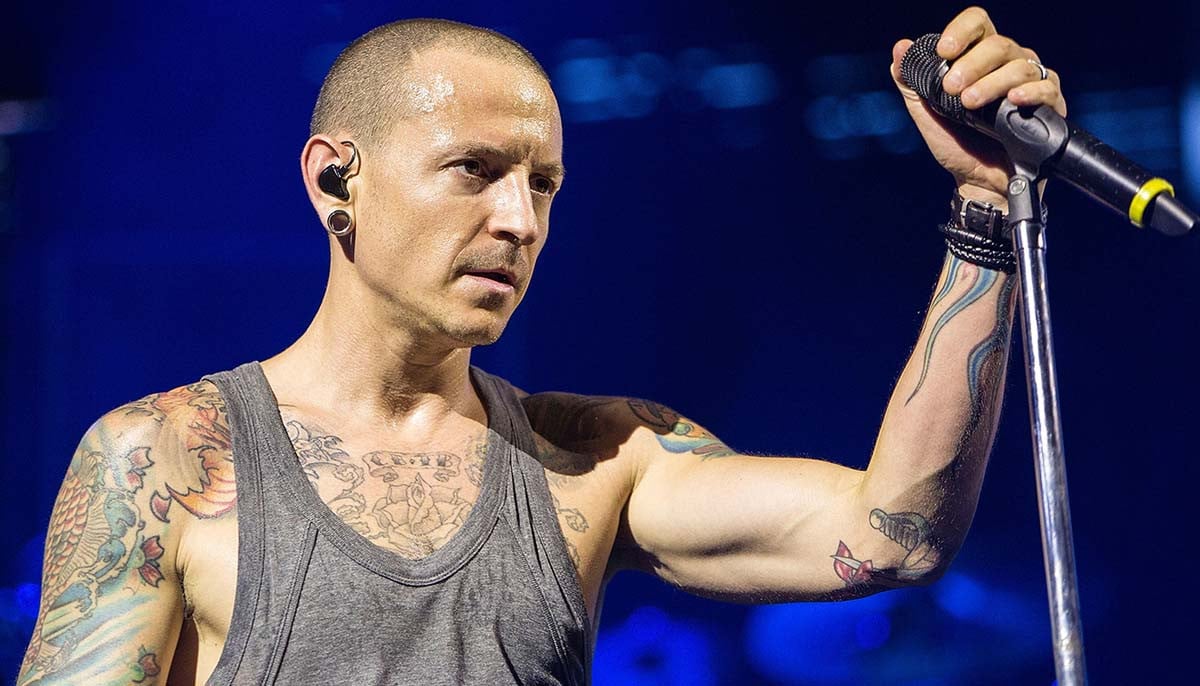
Chester Bennington’s mental health story and lasting legacy
-
Yerin Ha opens up about shocking diagnosis post ‘Bridgerton’ season 4
-
Everything to know about Justin Bieber's facial paralysis
-
Sarah Ferguson’s dual cancer journey
-
Demi Moore was left with ‘intense’ illness after ‘The Substance’
-
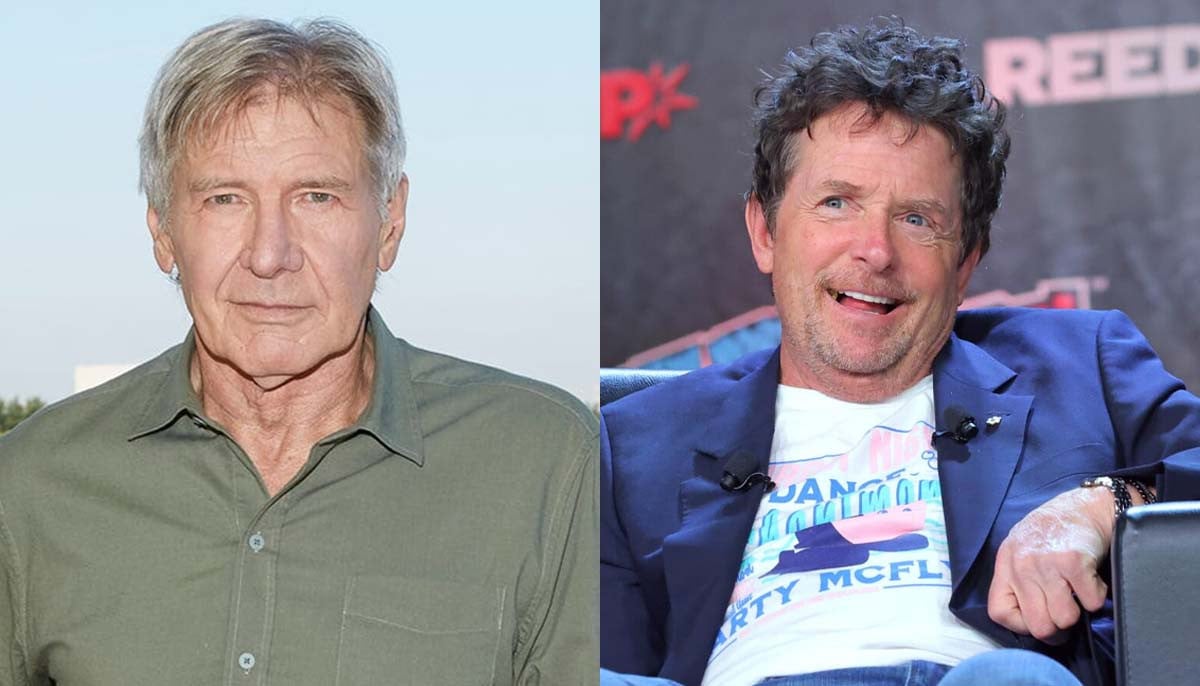
How Michael J. Fox helped Harrison Ford with his Parkinson's monologue