
India has achieved a milestone by becoming polio-free. But it was not an easy task, required highest level of political commitment, consistent efforts, and a broad vision.
This was possible "due to unwavering political will", "adequate financial resources", "technological innovation" and "efforts of millions of workers" (2.3 million), according to India’s Union Health Minister, Ghulam Nabi Azad.
Only four years ago, in 2009, India had reported 741 polio cases, according to the Global Polio Eradication Initiative. According to the Indian health ministry, India had the highest number of polio cases or half of the total cases around the world at that time. The last case was reported from the eastern state of West Bengal in 2011, when an 18-month-old girl was found to have contracted the disease.
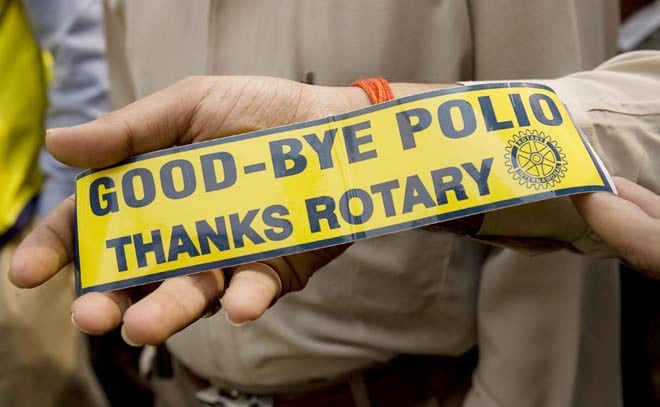
"Despite the obstacles, India proved to the world how to conquer this disease: through the government’s strong commitment, seamless partnership comprising the government, Rotary clubs, WHO and Unicef, and, above all, the tireless hard work of millions of front-line workers -- vaccinators, social mobilisers, and community and health workers," says Nicole Deutsch, head of polio operations in India for Unicef in a news report.
In a huge country like India, which is home to more than a billion people of cultural, economical, linguistic, and social diversity, it required projects adjustable to the local environment, such as micro-plans for each locality.
Vaccination against polio started in India in 1978 with Expanded Program in Immunisation (EPI). It was successful in covering about 40 per cent of all infants by 1984, giving three doses of OPV to each. In 1985, the Universal Immunisation Program (UIP) was launched to cover all districts of the country.
India’s concerted efforts to eradicate polio started in 1995 with Pulse Polio campaign. At the time, India had over 2,500 cases of polio per year. In 2002, special strategies to reach India’s under-served population were developed. Later on in 2004, new monovalent vaccines were introduced and, by 2007, efforts were focused on reaching mobile populations. Subsequently in 2009, the new bivalent vaccine was introduced to allow simultaneous targeting of the two remaining virus strains in a single vaccine. The World Health Organisation (WHO) removed India from the list of polio-endemic countries in 2012. The country completed two years without any case of polio on 13 January 2013.
India spends nearly one-tenth of its public outlay on health on the Pulse Polio campaign every year. The Indian government alone is reported to have spent over one billion US dollars for rooting out polio from its country. In addition to that, there was international assistance of an estimated equal amount.
It shows that the polio eradication strategies adopted by experts in India are effective in stopping polio even in the most challenging conditions.
And that is not all. India is committed to run polio campaigns in 2014 and 2015, planning six polio campaigns for the two years. As a precaution, it is reported to have set up polio immunisation posts along the international borders with Pakistan, Nepal, Bangladesh, Burma and Bhutan to vaccinate all children up to the age of five years, coming to India.
Experts warn that India’s proximity to Pakistan and Afghanistan and the fact that India had exported polio to countries such as Nepal, Tajikistan and Angola, still puts India at risk of polio virus importation.
There is still a risk of the polio virus making a comeback. Since 2000, as many as 44 countries that had been declared polio free have suffered from one or more importations of wild polio virus.
But this success comes with apprehensions about sustainability of the campaign, especially for all preventable diseases. The country lacks the resources for comprehensive preventive public health systems, including interventions in areas such as sanitation, drainage, potable water, health awareness campaigns, etc., which minimise citizens’ exposure to diseases. In high-risk states, such as Uttar Pradesh and Bihar, health staff spends as much as half of their working days in a year on the campaign at the cost of other interventions, which include routine immunisation and health check-ups.
For the time, India’s example is for the region’s countries to follow. "It sets the stage for the entire South East Asian region of WHO to be certified polio-free," says Sona Bari, spokesperson of WHO’s polio-eradication campaign, in an interview to Xinhua, adding, "The focus was not only on figuring out how to reach more than 172 million children under the age of five years with multiple doses of vaccine but also to do so in a manner that maximises the impact of each immunisation contact."
WHO has advised the government to take necessary precautions by seeking immunisation of incoming visitors from polio affected countries six weeks prior to their arrival in India and also to arrange Oral Polio Vaccination (OPV) for Indian citizens travelling to those countries.
Dr. Naveen Thacker, who was part of the team that led India’s eradication efforts, in an interview to India Ink in October 2012, ascribes this to "political support at every level of government". He says, "The government (had) set up the India Expert Advisory Group to ensure that we could identify and address challenges quickly and effectively."
Thacker says it was not just a professional but personal commitment too, "I got involved in polio eradication in 1994, when there was a polio outbreak in my home state of Gujarat, where I personally saw 55 cases in less than two months."
The resources were also made available. "The government of India and public-private partnerships together put in almost 1.5 billion dollars to the polio eradication campaign, combined with the partnership of Rotary International, the World Health Organization, Unicef, etc. In Bihar, and Uttar Pradesh, history was made by administering over 900 million doses of oral polio vaccine," he says proudly.
India also kept pace with the new technological advancements as "utilising new technological innovations was crucial to India’s eradication success," he says, adding, "For example, genetic sequencing helped us quickly identify where an outbreak of the virus had originated, so that we could prevent more polio cases. Furthermore, the new bivalent vaccine in 2008 meant children were better protected against polio and it cost less money."